The final calculated sample size after adding 10% non-respondents was 422.
Sampling techniques
There are eight government hospitals in the Wolaita zone. The total number of nurses who were involved in direct patient care in each hospital was, 480 in WSUCSH, 45 in Humbo Primary Hospital, 37 in Bodit Primary Hospital, 30 in Kindo Didaye Primary Hospital, 39 in Bitena Primary Hospital, 50 in Gesuba Primary Hospital, 42 in Bele Primary Hospial, and 55 in Bombe Primary Hospitals. A proportional size allocation was applied to each hospital, and we get a sample of 268 from WSUCSH, 25 from Humbo Primary Hospital, 21 from Bodit Primary Hospital, 16 from Kindo Didaye Primary Hospital, 22 from Bitena Primary Hospital, 28 from Gesuba Primary Hospital, 23 from Bele Primary Hospial, and 29 from Bombe Primary Hospitals. The nurses involved in direct patient care at each hospital were listed in a series of orders to create a sampling frame. Then a systematic random sampling technique with a sampling interval of 2 for each hospital was used to get the study participants, and random start 1 was determined by lottery.
Data collection tools, procedures and data collectors
A self-administered, structured questionnaire was used to collect the data. The questionnaire was prepared by reviewing different literature [1, 17]. Twenty-two questions, divided into four domains (physiological, psychological, sociocultural, and spiritual), were used to evaluate holistic nursing care practice. The participants’ knowledge level was measured by eight measuring items. Knowledge level was scored by the proportion of correctly answered items. The mean was calculated, and those who answered above the mean were regarded as having good knowledge, and respondents who answered knowledge-related questions below the mean value were regarded as having poor knowledge [17]. The condition of the patient was described based on American Hospital Association guidelines [18]. A total of eight BSc nurses’ and four supervisors with MSc qualifications were involved in the data collection process. The data collectors distribute the questionnaire after explaining the purpose and technique of filling it out, and then collect the questionnaire back.
Operational definitions
Good practice in each domain
The respondent who answered a practice-related question in the given domain above the mean [17].
Poor practice in each domain
The respondent who answered a practice-related question in the given domain below the mean [17].
Good holistic nursing care practice
The respondent who fulfilled all domains of holistic nursing care practice [19, 20].
Poor holistic care practice
The respondent who missed at least one domain of holistic care practice [19, 20].
Good knowledge: The respondent who scored above the mean [17].
Poor knowledge level
The respondent who scored below the mean [17].
Good relationship
Respondents who answered the relationship-related question above the mean value [1].
Poor relationship
Respondents who answered the relationship-related question below the mean value [1].
Job satisfaction
When the total score for the job satisfaction subscale was greater than the computed mean, they were satisfied with the overall aspect of their work [21].
The condition of the patient Was described based on the American Hospital Association guidelines as.
- Good: Vital signs are stable and within normal limits. The patient is conscious and comfortable. Indicators are excellent.
- Fair: Vital signs are stable and within normal limits. The patient is conscious but may be uncomfortable. Indicators are favorable.
- Serious: Vital signs may be unstable and not within normal limits. The patient is acutely ill. Indicators are questionable.
- Critical: Vital signs are unstable and not within normal limits. The patient may be unconscious. Indicators are unfavorable [18].
Data quality control
To maintain the quality of the data, two days of training were given to data collectors and supervisors by the principal investigator on the data collection tools and procedures. A pre-test was conducted on 5% of the sample size before actual data collection in Tercha General Hospital, Dawuro Zone. The reliability of the tool was checked by calculating a Cronbach’s Alpha of 89.7%. Close follow-up and supervision were conducted during the data collection period. The collected data were checked by supervisors every day.
Data analysis
The collected data was checked for its completeness, then coded, and the data was entered using Epi Data version 4.6 and analyzed using SPSS version 25. Descriptive statistics were used to describe each individual variable using the frequency distribution, percentage, mean, and standard deviation. A binary logistic regression analysis was computed for each predictor variable in holistic nursing care. Then variables with a p value less than 0.25 were entered into the multivariable logistic regression analysis. Both crude odd ratios (COR) and adjusted odd ratios (AOR) with 95% CI were used to identify predictor variables. Variables that had a p-value less than 0.05 were considered significant.
Ethical consideration
The research was approved by the Ethical Review Committee of Wolaita Sodo University College of Health Science and Medicine. An official letter was written to each hospital director. All methods were carried out in accordance with the Declaration of Helsinki and its later amendments or comparable ethical standards. All study participants were encouraged to participate in the study, and at the same time, the data collectors told the participants that they had the right not to participate. Finally, data was collected after assuring the confidentiality of responses and obtaining written informed consent from the study participants.
Results
Socio-demographic characteristics
A total of 391 participants were included in the study, with a response rate of 92.65%. The majority of respondents, 220 (56.3%), were male, and one hundred eighty-one (46.3%) of the nurses were in the age category between 25 and 30 years, with a mean ± SD age of 29 ± 5.9 years. Two hundred fifteen (55%) of respondents were married, and three hundred seven (78.5%) of the nurses had a BSc degree or above, and 237 (60.6%) had less than 5 years of experience, with a mean ± SD of work experience of 5.3 ± 4.3 years. Ninety-nine (25.3%) of the respondents were from the medical ward (Table 1).
Nurse related factors
Two hundred thirty-nine (61.1%) of the nurses had good knowledge of holistic nursing care. One hundred eighty-seven (47.8%) of the nurses had a good relationship with patients, and 209 (53.5%) were satisfied with their jobs (Table 3).
Table 3 Nurse related factors of respondents in public hospitals of Wolaita Zone, South Ethiopia, 2022
Factors associated to holistic nursing care of the respondents
Ten variables were selected as candidate variables out of 19 independent variables for multiple logistic regression analysis. In multivariable logistic regression, five variables (nurse’s level of education, ward or unit of work, continuous in-service learning, nurse-patient relationship, and knowledge level of nurses) were found to be significantly associated with holistic nursing care practice.
Nurses who had a diploma in nursing were 72% less likely to practice holistic nursing care than nurses who had a BSc. Degree or higher in nursing (AOR = 0.28; 95% CI: 0.11, 0.71). Nurses working in ICU were 78% (AOR = 0.22; 95% CI: 0.07, 0.69); Gynecological wards were 71% (AOR = 0.29; 95% CI: 0.10, 0.82); Pediatric wards were 86% (AOR = 0.14; 95% CI: 0.04, 0.44); and Nurses who were working in other wards (such as ophthalmological, dialysis, oncologic, psychiatric, and orthopedic wards) were 71% (AOR = 0.29; 95% CI: 0.13, 0.65) less likely to practice holistic nursing care compared to nurses who were working in the medical ward.
Nurses who were working in the hospital where there was no continuous in-service learning were 61% (AOR = 0.39; 95% CI: 0.20, 0.76) less likely to practice holistic nursing care compared to those working in the hospital where there was continuous in-service learning.
Nurses who had a poor relationship with patients were 69% (AOR = 0.31; 95% CI: 0.16, 0.58) less likely to practice holistic nursing care compared to those nurses who had a good relationship with patients.
Nurses who had poor knowledge of holistic nursing care practice were 59% (AOR = 0.41; 95% CI: 0.21, 0.79) less likely to practice holistic nursing care compared to those nurses who had good knowledge (Table 4).
Table 4 Factors associated with Holistic Nursing care practice among nurses in public hospitals of Wolaita Zone, South Ethiopia, 2022
Discussions
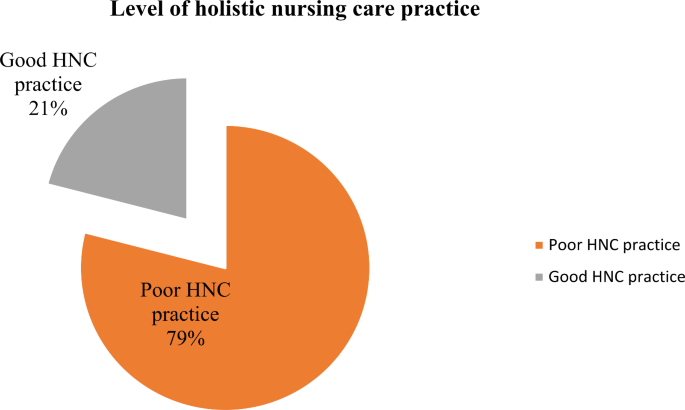
This study revealed that 21.0% (95% CI: 17.6, 25.1) of nurses practiced all the components of holistic nursing care. Nurses level of education, ward or unit of work, continuous in-service learning, nurse-patient relationship, and knowledge level on holistic nursing care were found to be the factors associated with holistic nursing care practice.
Nurses practiced individual components of holistic nursing care; however, the overall holistic nursing care practice of the individual nurse was 21.0% (95% CI: 17.6, 25.1). This might be due to nurses focus on individual components of patients rather than addressing patient needs holistically [11] or the lack of a comprehensive guide to practicing holistic nursing care in hospitals [23]. [23].
The individual components as well as the overall practice of holistic nursing care in our study were lower than in the study conducted in Cameroon, which found that 28.6% of the nurses based their practice on the biological aspect, 18.6% on the psychological aspect, 27.1% on the social aspect, 14.3% on the spiritual aspect, and 11.14% truly practiced all of the aspects [24]. This difference might be due to the socio-demographic differences among nurses or the differences in resources allocated for the health care systems in the two countries.
The study results showed that 61% of nurses had knowledge of holistic nursing care. This finding supported the study conducted in Kenya, which showed that nurses keep their knowledge of holistic care up-to-date but are unable to transfer their theoretical knowledge into the practice of holistic nursing care. This might be due to a lack of in-service training in the provision of holistic nursing care. There must be adequate time, knowledge, motivation, and training given to nurses at all levels of health institutions in order to provide holistic care for patients [1].
It was observed that nurses who had a diploma in nursing were 72% less likely to practice holistic nursing care than nurses who had a BSc. Degree or above in nursing (AOR = 0.282; 95% CI: 0.113, 0.709). This finding is consistent with cross-sectional studies conducted in Malaysia and Turkey [25, 26], [25,26,27] which conclude that better education and training for nurses are required for satisfying clients and sustaining the outcomes of patient care. This finding is also in line with the former study, which concluded that a lack of education affects clinical practice [28]. This might be due to the fact that nurses with a lower educational level might be less exposed to the concept of holistic nursing care and practice. The information gap might have helped them understand the purpose and importance of HNC, which may have influenced their practice. A lack of opportunity for education can hinder the provision of holistic care [22].
Accordingly, nurses who had worked in a hospital in which there was no continuous in-service learning were 61% less likely to practice holistic nursing care than those who had worked in a hospital in which there was continuous in-service learning (AOR = 0.39; 95% CI: 0.20, 0.76). This finding was consistent with a former study done in Iran, which implied that nurses would provide holistic care if educators provided holistic care in a practical model [11]. The study conducted in India was also consistent with this finding, which resulted in a mismatch between academic learning and clinical performance that can hinder the provision of holistic nursing care [29]. Additionally, the former qualitative study conducted in South Africa indicated that the need for continuous in-service education on different topics had an impact on holistic care [30]. This might be due to the fact that [30] nurses with lower awareness regarding holistic nursing care may not be able to understand the purpose and importance of HNC, which might affect their HNC practice.
Nurses who had a poor relationship with patients were 69% less likely to practice holistic nursing care than those who had a good relationship with patients (AOR = 0.31; 95% CI: 0.16–0.58). This result was in line with the study conducted in Kenyatta’s national hospital, which indicated that the interpersonal relations and rapport between the nurses and the patients can directly affect the holistic care provision [1]. This finding supports a qualitative study conducted in South Africa, which recommended that demonstrating companionship and respect for the patient were important during holistic care [30]. This is also in line with Watson’s theory of human caring, which places emphasis on cultivating and maintaining caring and helpful relationships [31]. The qualitative study also supported this finding by stating that there should be humanity in caring for patients, a desire to maintain helpful relationships, and love and kindness for patients in order to provide holistic nursing care. This might be due to the fact that nurses who are social and emotionally stable are more capable of identifying the needs of patients [29] and providing care accordingly.
Nurses who had poor knowledge of holistic nursing care practice were 59% less likely to practice holistic nursing care than those with good knowledge (AOR = 0.41; 95% CI: 0.21, 0.79). The study conducted in South Africa [30], and Kenya [1], and Saudi Arabia [12] supported this finding. This might be due to an in-depth knowledge of holistic care that increases the nurse’s provision of care, or it might be due to knowledge and evidence used in practice that raises awareness of professional and personal accountability and the dilemmas of practice, which improves care [30, 32]. The mixed-type study done in Kenya was consistent with this finding, which indicated that the knowledge base of the nurses concerning the care they provide can affect the provision of holistic care [1]. Additionally, this finding also supported the study conducted in Saudi Arabia, which concluded that to provide patients with holistic care, nurses must be knowledgeable in the holistic approach [12] .
Conclusions
Holistic nursing care practice was low among nurses, according to this study. Lower levels of education, the unit of work, a lack of continuous in-service learning, a poor nurse-patient relationship, and the poor knowledge level of nurses on holistic nursing care were factors associated with the practice of holistic nursing care. Therefore, the provision of in-service training is suggested to improve the knowledge and practice of holistic nursing care. Moreover, encouraging and motivating nurses to properly provide HNC for patients should be emphasized in public hospitals.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.